Abstract
Red Blood Cell Adhesion in Adult Patients with Sickle Cell Disease, at Baseline and with Pain, Measured on SCD Biochip Microfluidic Assay
Alexandra Boye-Doe1, Erina Quinn1, Charlotte Yuan1, Umut A. Gurkan, PhD1, and Jane A. Little, MD2
1Case Western Reserve University, Cleveland, OH; 2Division of Hematology/Oncology, Case Western Reserve University/ University Hospitals Seidman Cancer Center, Cleveland, OH
Background:
Despite being monogenic, sickle cell disease (SCD) has a variable phenotype, in which clinical complications and manifestations evolve as patients age. In children, pain generally resolves between crises, whereas adults may experience acute, chronic, or acute-on-chronic pain. We have taken a multifaceted approach to characterize adhesion and inflammation during self-identified pain episodes in adults with SCD in order to better understand pain syndromes in adults and the potential for more specifically targeted therapies. In this pilot study, we assessed changes in red blood cell (RBC) adhesion to the subendothelial protein laminin (LN) during crisis in adults with SCD self-reporting for pain crisis on whom we had baseline adhesion data from a routine clinic visit.
Methods:
Surplus blood from patients' routine bloodwork was used. Crisis samples were collected from patients at the Acute Care Clinic or Emergency Department at University Hospitals Cleveland Medical Center (UHCMC) when patients presented for management of pain. Baseline samples were collected during routine visits to the Sickle Cell Clinic. This study was approved by the IRB at UHCMC. Within a 24-hour period, RBC adhesion to LN was quantitated by microscopy after passage of unprocessed whole blood through a LN-coated microfluidic adhesion assay, the SCD biochip [1]. Samples were analyzed for hemoglobin (Hb) phenotype by high-performance liquid chromatography (HPLC) in the clinical lab. Correlative clinical data, including, baseline lab values, and medical history, were obtained from the patients' medical records and used to characterize our results. Data from people with multiple samples were used as median values.
Results:
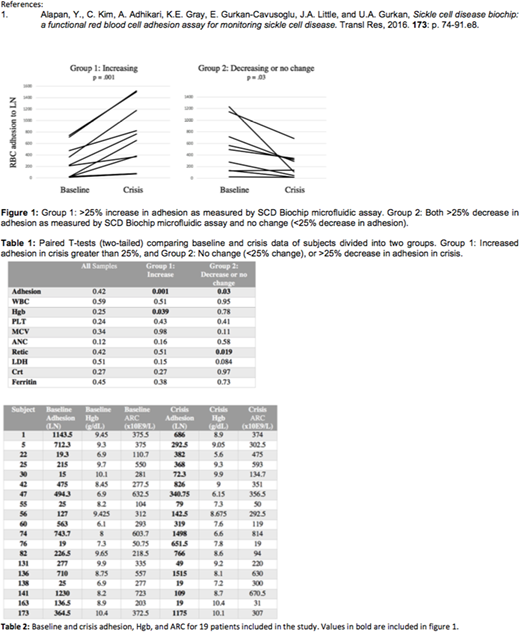
Blood samples from 19 unselected patients with sickle cell hemoglobin SS (HbSS) were obtained at crisis, and compared with baseline samples obtained from 2014 to 2018 (n = 67 samples). 2 groups were identified: Group 1 with increased adhesion (>25% rise from baseline, n= 10) during crisis, and Group 2 with decreased adhesion (>25% fall from baseline, n=8) or no change (<25% change) (n=1) during crisis (Fig. 1). Time between a patient's initial crisis event and when they presented for pain management varied, possibly affecting observed adhesion. Nonetheless, patients showing an increased adhesion in crisis also showed a decrease in Hb (p = 0.039) between their baseline analyses and the crisis visit. A decrease in Hb may associate with increased adhesion, if the latter contributes to crisis-related hemolysis. However, other markers of hemolysis did not change. By contrast, patients with decreasing RBC adhesion showed a decrease in absolute reticulocyte count (ARC, p = 0.019) at their crisis visit. Statistical analysis of HbS, HbA, and HbF levels n = 64 showed no significant change between baseline or crises.
Discussion:
A decrease in adhesion during crisis may reflect the presence of sickled RBCs that adhere preferentially to other basement membrane proteins such as fibronectin or thrombospondin. In addition, inflammatory white blood cell adhesion, possibly central to vaso-occlusion, is not evaluated in this study. We are currently examining cytokine and monocyte profiles from people with SCD presenting for management of pain, so that we may better understand inflammatory mediators of pain. Our data are the first to try to understand RBC adhesion in people with SCD who present for management of pain, whether this as an isolated or common event for that person. We found that unselected adults with SCD who presented for management of pain had heterogeneous changes in RBC adhesion, which may reflect differences in underlying mechanism. The pathophysiologic heterogeneity of pain in adults with SCD will be important to understand as anti-adhesion therapies are being developed and adopted clinically.
Little:Doris Duke Charitable Foundations: Research Funding; NHLBI: Research Funding; Hemex: Patents & Royalties: Patent, no honoraria; PCORI: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal